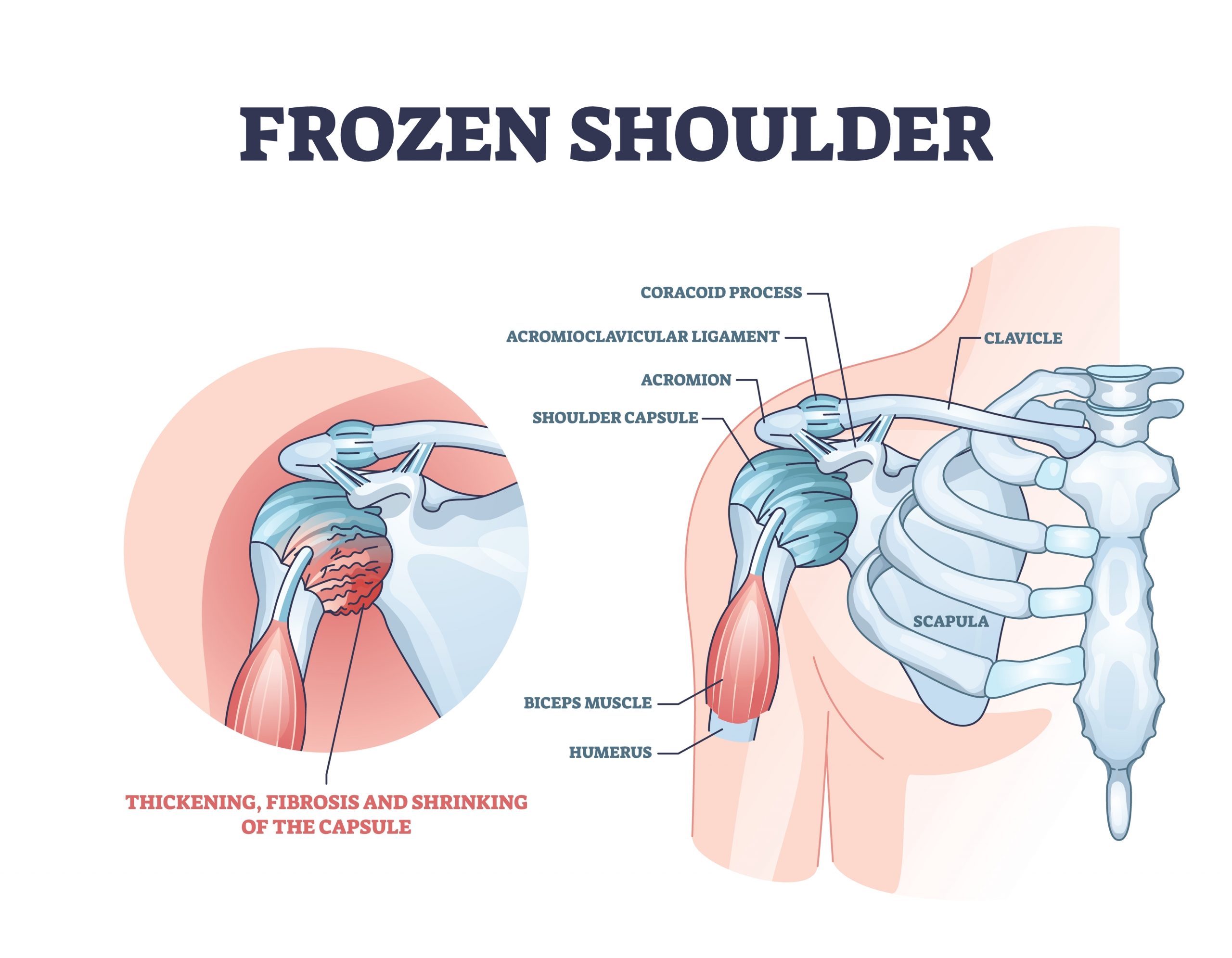
Frozen shoulder, medically called adhesive capsulitis, is a condition that causes stiffness, pain, and limited movement in the shoulder joint. It can significantly affect daily activities, making simple tasks like reaching, lifting, or dressing challenging. Early diagnosis and treatment are essential for restoring shoulder mobility and preventing long-term complications.
What is Frozen Shoulder?
The shoulder joint is a ball-and-socket joint, surrounded by a capsule of connective tissue. In frozen shoulder:
-
The capsule becomes inflamed and stiff.
-
Scar tissue (adhesions) develops inside the capsule.
-
The shoulder loses its normal range of motion, making movement painful.
Frozen shoulder typically progresses in three stages:
-
Freezing Stage: Gradual onset of pain and stiffness, lasting 6–9 months.
-
Frozen Stage: Pain may decrease, but stiffness remains, lasting 4–6 months.
-
Thawing Stage: Gradual improvement in mobility, often taking 6 months to 2 years.
Causes of Frozen Shoulder
Frozen shoulder can occur without a clear cause (idiopathic) or secondary to other conditions. Common causes include:
1. Injury or Surgery
Immobilization of the shoulder after fractures, rotator cuff injuries, or surgery can trigger stiffness and adhesive capsulitis.
2. Diabetes
People with diabetes have a higher risk of developing frozen shoulder, and recovery may take longer.
3. Other Medical Conditions
-
Thyroid disorders (hypothyroidism or hyperthyroidism)
-
Cardiovascular disease
-
Parkinson’s disease
4. Age and Gender
Frozen shoulder most commonly affects adults aged 40–60, with women being slightly more prone than men.
Symptoms of Frozen Shoulder
Frozen shoulder symptoms develop gradually and can vary in intensity:
-
Pain: Often dull or aching, worsens at night or with movement.
-
Stiffness: Difficulty lifting the arm overhead or behind the back.
-
Reduced Range of Motion: Movements such as reaching, combing hair, or dressing become challenging.
-
Weakness: Secondary to limited mobility and disuse.
Symptoms typically worsen during the freezing stage and slowly improve during the thawing stage.
Diagnosis
Diagnosing frozen shoulder involves a combination of medical history, physical examination, and sometimes imaging tests:
Physical Examination
-
Assessment of active and passive shoulder movements.
-
Checking for pain, stiffness, and limitations in rotation and abduction.
Imaging Tests
-
X-rays: Rule out arthritis, fractures, or other bone problems.
-
MRI: Evaluates the soft tissues, including the joint capsule and rotator cuff.
-
Ultrasound: Can detect inflammation and tendon issues.
Early diagnosis is key to initiating appropriate treatment and preventing prolonged disability.
Treatment Options
Treatment focuses on pain relief and restoring shoulder mobility. Most patients improve with conservative management, while severe cases may require surgical intervention.
1. Conservative Treatments
a) Physical Therapy
-
Stretching and strengthening exercises help restore motion.
-
Range-of-motion exercises like pendulum swings and wall climbs are commonly used.
-
Supervised therapy ensures safe progression and reduces the risk of further injury.
b) Medications
-
Pain relievers: Acetaminophen or NSAIDs help reduce pain and inflammation.
-
Topical analgesics: Creams or gels applied to the shoulder for localized relief.
c) Heat and Cold Therapy
-
Cold packs: Reduce inflammation during the early painful stage.
-
Heat therapy: Relaxes muscles and improves blood flow during stretching exercises.
d) Corticosteroid Injections
-
Reduce inflammation and pain in the shoulder capsule.
-
Often combined with physical therapy for better outcomes.
2. Surgical Treatments
Surgery is rarely needed and is considered if conservative treatment fails after 6–12 months:
-
Manipulation under anesthesia (MUA): The shoulder is gently moved to break adhesions while the patient is under anesthesia.
-
Arthroscopic Capsular Release: Minimally invasive procedure to cut tight portions of the capsule and restore motion.
Recovery and Prognosis
Recovery from frozen shoulder can be slow, often taking 12–24 months. Factors affecting recovery include:
-
Age and overall health
-
Presence of diabetes or other medical conditions
-
Adherence to physical therapy and exercises
Most patients regain near-normal shoulder function, although some may experience mild stiffness for years.
Prevention of Frozen Shoulder
While not all cases can be prevented, the risk can be reduced with the following strategies:
-
Early Mobilization: Move the shoulder gently after injury or surgery.
-
Regular Exercise: Maintain shoulder flexibility and strength.
-
Manage Medical Conditions: Properly control diabetes and thyroid disorders.
-
Avoid Prolonged Immobilization: Use supports or slings only as advised by a doctor.
Conclusion
Frozen shoulder is a painful condition that can significantly impact daily life. Early recognition, physical therapy, and medical management can speed recovery and restore shoulder function. Most patients recover fully with proper care, though patience is necessary due to the gradual nature of healing.
If you experience persistent shoulder pain or stiffness, consulting an orthopaedic specialist is crucial for proper evaluation and treatment.