The spine is one of the most crucial parts of our body, providing structural support, flexibility, and protection for the spinal cord. However, with the demands of modern life, such as prolonged sitting, heavy lifting, and sedentary lifestyles, spinal problems are becoming increasingly common. One of the most prevalent spine issues is a slipped disc, also known as a herniated disc.
In this blog, we will explore what a slipped disc is, its causes, symptoms, and the available treatment options.
What is a Slipped Disc?
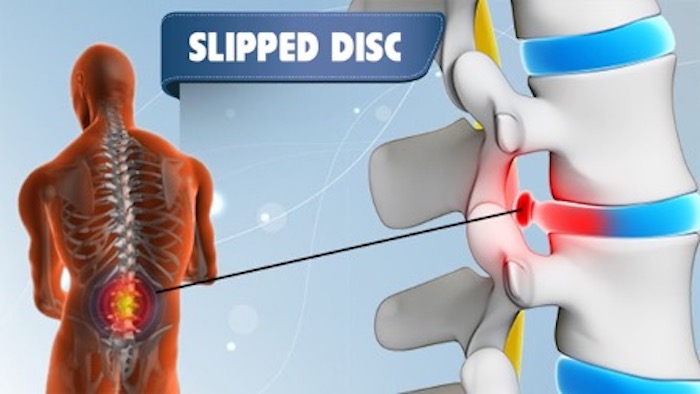
The human spine is made up of 33 vertebrae stacked on top of each other, separated by intervertebral discs. These discs act as shock absorbers, cushioning the spine during movement. Each disc has two parts:
-
Nucleus pulposus: The soft, jelly-like inner core.
-
Annulus fibrosus: The tough, outer layer that surrounds the nucleus.
A slipped disc occurs when the nucleus pulposus pushes out through a tear in the annulus fibrosus. This can irritate the nearby nerves and lead to pain, numbness, or weakness in different parts of the body depending on the location of the herniation.
Causes of Slipped Disc
A slipped disc can develop due to a combination of age-related wear and tear, lifestyle factors, and sudden injuries. The most common causes include:
1. Age-Related Degeneration
As we age, our spinal discs gradually lose water content and elasticity. This natural degeneration weakens the discs, making them more prone to herniation. Most cases occur in people aged 30 to 50 years.
2. Poor Posture
Long hours of sitting, especially with a slouched posture, increase the pressure on the spine. Poor posture can accelerate disc degeneration and increase the risk of a slipped disc.
3. Heavy Lifting and Sudden Movements
Improper lifting techniques, such as bending from the waist instead of the knees, can place extreme stress on the spinal discs. Twisting while lifting heavy objects can also trigger a herniation.
4. Obesity
Excess body weight increases stress on the lumbar spine, contributing to disc problems. Maintaining a healthy weight is essential to reduce the risk.
5. Sedentary Lifestyle
A lack of regular exercise weakens the muscles that support the spine. Strong core muscles help stabilize the spine and reduce the risk of disc herniation.
6. Smoking
Smoking reduces blood flow to the spinal discs, slowing down the natural healing process and accelerating degeneration.
7. Trauma or Injury
A fall, car accident, or sports injury can sometimes cause sudden disc herniation, especially if the spine is twisted or compressed.
Symptoms of a Slipped Disc
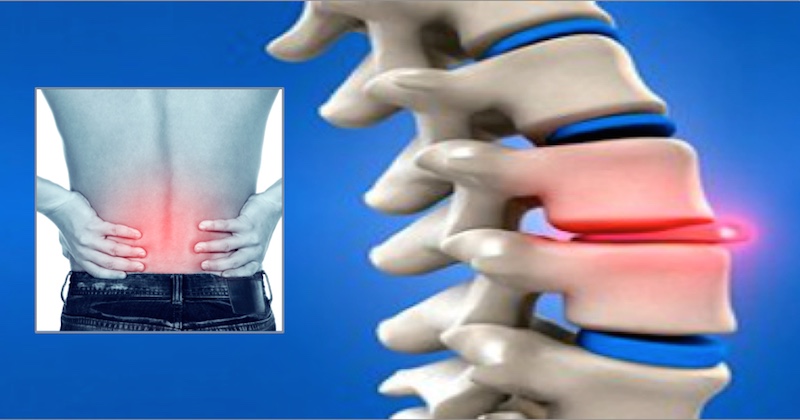
The symptoms of a slipped disc vary depending on the location and severity of the herniation. The most commonly affected areas are the lower back (lumbar spine) and the neck (cervical spine).
1. Lower Back (Lumbar Herniated Disc)
-
Lower back pain that worsens with movement, coughing, or sneezing.
-
Leg pain (sciatica): Sharp or burning pain radiating down one leg.
-
Numbness or tingling in the leg or foot.
-
Muscle weakness in the leg, making walking or standing difficult.
2. Neck (Cervical Herniated Disc)
-
Neck pain that may radiate to the shoulders and arms.
-
Arm pain or numbness in the hand or fingers.
-
Weak grip strength due to nerve compression.
-
Headaches in some cases.
3. Rare but Serious Symptoms
-
Loss of bladder or bowel control – this may indicate cauda equina syndrome, a medical emergency.
-
Severe weakness in the legs or arms.
If you experience any of these symptoms, it is crucial to seek medical attention immediately.
Diagnosis of a Slipped Disc
Diagnosing a slipped disc involves a combination of physical examination, medical history, and imaging studies.
1. Physical Examination
A doctor may check for:
-
Reflexes, muscle strength, and sensation.
-
Pain triggered by specific movements.
-
Ability to walk on toes or heels.
2. Imaging Tests
-
X-rays: Help rule out other spinal problems but cannot confirm a herniated disc.
-
MRI (Magnetic Resonance Imaging): The most effective test for detecting a herniated disc and nerve compression.
-
CT Scan: Sometimes used if MRI is not possible.
-
Myelogram: Rarely used, involves injecting contrast dye into the spinal canal.
Treatment Options for Slipped Disc
Treatment depends on the severity of the symptoms. Most cases improve with conservative treatment, while severe or persistent cases may require surgery.
1. Conservative Treatments
a) Rest and Activity Modification
Short-term rest can reduce inflammation, but prolonged bed rest is not recommended. Gentle movements and avoiding heavy lifting are advised.
b) Medications
-
Pain relievers: Such as acetaminophen or NSAIDs (ibuprofen).
-
Muscle relaxants: To reduce muscle spasms.
-
Nerve pain medications: Like gabapentin for severe nerve-related pain.
c) Physical Therapy
A physical therapist can design exercises to:
-
Strengthen core muscles.
-
Improve flexibility and posture.
-
Reduce pressure on the affected disc.
d) Hot and Cold Therapy
-
Cold packs: Reduce inflammation and numb acute pain.
-
Heat therapy: Relaxes muscles and improves blood flow.
e) Epidural Steroid Injections
For severe pain not relieved by medications, corticosteroid injections around the affected nerve can reduce inflammation and pain.
2. Surgical Treatments
Surgery is considered only if:
-
Pain persists for 6–12 weeks despite conservative treatment.
-
There is significant weakness, numbness, or nerve compression.
-
Loss of bladder or bowel control occurs.
Common surgical options include:
a) Discectomy
The surgeon removes the herniated portion of the disc to relieve nerve pressure.
b) Microdiscectomy
A minimally invasive version of discectomy using small incisions and a microscope.
c) Laminectomy
Removal of a small portion of the vertebral bone to relieve pressure on the nerve.
d) Spinal Fusion
In severe cases, two vertebrae may be fused to stabilize the spine.
Prevention of Slipped Disc
Prevention is always better than cure. Here are some effective strategies:
-
Maintain Good Posture: Sit and stand with a straight spine.
-
Exercise Regularly: Focus on core strengthening, flexibility, and aerobic exercises.
-
Lift Correctly: Bend your knees, not your waist, and avoid twisting.
-
Maintain Healthy Weight: Reduce pressure on your spine.
-
Avoid Smoking: Promotes disc health.
-
Stay Active: Avoid long periods of sitting; take breaks to stretch.
When to See a Doctor
Seek medical help if you experience:
-
Persistent back or neck pain.
-
Numbness, tingling, or weakness in limbs.
-
Pain radiating down the leg or arm.
-
Loss of bladder or bowel control (emergency).
Early diagnosis and treatment can prevent complications and improve recovery.
Recovery and Prognosis
Most people with a slipped disc respond well to conservative treatment and recover within 6–12 weeks. Surgery is highly effective for severe cases, with many patients returning to normal activities within a few months.
Lifestyle changes, proper posture, and regular exercise play a crucial role in preventing recurrence.
Conclusion
A slipped disc is a common spinal problem that can significantly affect your quality of life if left untreated. Understanding the causes, symptoms, and treatment options can help you take proactive steps toward recovery. With timely medical intervention, physical therapy, and lifestyle modifications, most patients experience significant relief and return to their daily activities.
If you are experiencing persistent back or neck pain, consulting a spine specialist is essential. Early diagnosis not only prevents complications but also ensures a faster and more effective recovery.