Rheumatoid Arthritis (RA) is one of the most common and challenging autoimmune disorders, affecting millions of people worldwide. Unlike ordinary joint pain or age-related arthritis, RA is a chronic inflammatory disease where the body’s immune system mistakenly attacks its own joints. This abnormal response leads to persistent pain, swelling, stiffness, and potential damage to multiple organs if not managed properly.
In this comprehensive blog, we will explore what rheumatoid arthritis is, its causes, symptoms, risk factors, complications, and available treatment options, while also focusing on lifestyle strategies that can help patients live healthier lives.
What is Rheumatoid Arthritis?
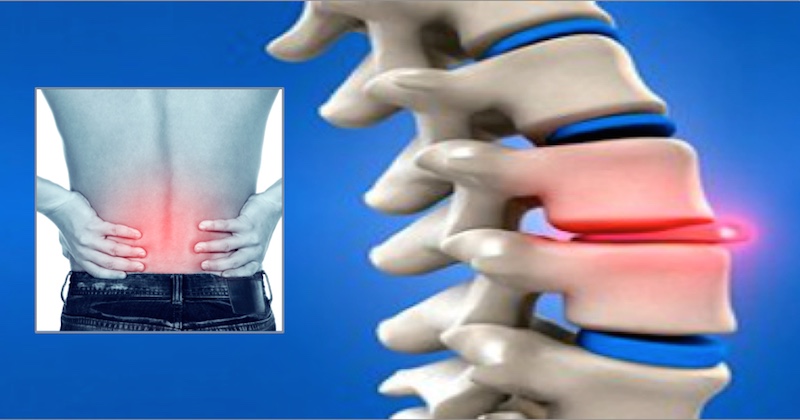
Rheumatoid Arthritis is a chronic autoimmune disorder in which the immune system mistakenly attacks the synovium—the lining of the membranes surrounding the joints. This causes inflammation, which can eventually damage cartilage, bone, and surrounding ligaments. Unlike osteoarthritis, which is caused by wear and tear, RA is a systemic disease that can affect not only joints but also organs like the lungs, heart, skin, and eyes.
RA typically starts in small joints (like fingers and toes) but can spread to larger joints such as knees, shoulders, and hips. It often occurs symmetrically—if one knee is affected, the other is likely to be affected too.
The Autoimmune Connection
The immune system is designed to protect the body from harmful invaders such as bacteria and viruses. In RA, however, this system becomes overactive and mistakenly identifies healthy tissues in the joints as foreign. The white blood cells release chemicals that cause inflammation, resulting in swelling, pain, and eventually joint damage.
The exact trigger for this autoimmune reaction is still unclear, but researchers believe that a combination of genetics, environmental factors, and hormonal influences plays a role.
Causes and Risk Factors
Though the exact cause of RA is unknown, certain factors increase the risk of developing it:
-
Genetics – Family history plays a role. People with certain genes (like HLA-DR4) are more prone to RA.
-
Gender – Women are two to three times more likely to develop RA than men.
-
Age – While RA can occur at any age, it most commonly develops between the ages of 30 and 60.
-
Smoking – Cigarette smoking is one of the strongest modifiable risk factors linked to RA.
-
Obesity – Excess body weight increases stress on joints and may promote inflammation.
-
Hormonal factors – Changes in female hormones, especially after pregnancy or menopause, may trigger RA.
-
Environmental factors – Exposure to pollutants, silica dust, and infections may contribute to RA onset.
Symptoms of Rheumatoid Arthritis
RA symptoms can vary in severity and may come and go, but the hallmark features include:
1. Joint Symptoms
-
Pain and swelling in multiple joints.
-
Stiffness, especially in the morning or after inactivity (lasting more than 30 minutes).
-
Warmth and redness around affected joints.
-
Symmetry—the same joints on both sides of the body are affected.
2. General Symptoms
-
Fatigue and low energy.
-
Mild fever.
-
Loss of appetite.
-
Weight loss.
3. Advanced Symptoms
-
Joint deformities and loss of function.
-
Nodules (firm lumps under the skin near affected joints).
-
Inflammation in organs like eyes, heart, lungs, and blood vessels.
Stages of Rheumatoid Arthritis
RA progresses through different stages:
-
Early Stage – Inflammation of the synovium, causing mild symptoms like stiffness and joint pain.
-
Moderate Stage – Inflammation begins to damage cartilage, leading to reduced joint mobility.
-
Severe Stage – Damage extends to bones, causing deformities and severe pain.
-
End-Stage – Loss of joint function, possible disability, and damage to internal organs.
Diagnosis of Rheumatoid Arthritis
Diagnosing RA can be challenging, especially in its early stages, because symptoms may mimic other conditions. A rheumatologist usually conducts the following:
-
Medical history and physical exam – Checking joint swelling, tenderness, and movement.
-
Blood tests –
-
Rheumatoid Factor (RF)
-
Anti-CCP (anti-cyclic citrullinated peptide antibodies)
-
ESR (Erythrocyte Sedimentation Rate)
-
CRP (C-Reactive Protein)
-
-
Imaging tests – X-rays, ultrasound, or MRI to assess joint damage.
Early diagnosis is crucial because joint damage begins within the first few months of disease onset.
Complications of Rheumatoid Arthritis
If untreated or poorly managed, RA can lead to serious complications:
-
Joint deformities and disability
-
Cardiovascular diseases (increased risk of heart attack and stroke)
-
Lung problems (inflammation and scarring)
-
Eye issues (dry eyes, scleritis)
-
Osteoporosis (weak bones due to inflammation and medications)
-
Rheumatoid nodules (lumps under the skin)
-
Mental health issues like depression and anxiety due to chronic pain and disability
Treatment Options for Rheumatoid Arthritis
While there is no permanent cure for RA, effective treatments can control symptoms, slow progression, and improve quality of life. Treatment strategies include:
1. Medications
-
Disease-Modifying Antirheumatic Drugs (DMARDs) – e.g., Methotrexate, Sulfasalazine, Leflunomide. These slow disease progression.
-
Biologic Agents – e.g., TNF inhibitors, Interleukin inhibitors, and JAK inhibitors. Target specific parts of the immune system.
-
NSAIDs (Nonsteroidal Anti-Inflammatory Drugs) – Provide pain relief and reduce inflammation.
-
Corticosteroids – Used for quick symptom relief in flare-ups but not recommended for long-term use.
2. Physical Therapy
Exercises that improve joint flexibility, strength, and posture. Occupational therapy may also help in adapting daily activities.
3. Lifestyle Modifications
-
Regular low-impact exercise (yoga, swimming, cycling).
-
Balanced diet rich in anti-inflammatory foods.
-
Adequate sleep and stress management.
-
Avoiding smoking and alcohol.
4. Surgery
For severe joint damage, surgical options like joint replacement, tendon repair, or synovectomy may be considered.
Diet and Nutrition in Rheumatoid Arthritis
Nutrition plays an important role in managing RA symptoms:
-
Anti-inflammatory foods: Fatty fish (salmon, tuna), flaxseeds, walnuts.
-
Fruits and vegetables: Rich in antioxidants like vitamins C and E.
-
Whole grains: Oats, quinoa, and brown rice reduce C-reactive protein (CRP) levels.
-
Legumes: Good source of protein and fiber.
-
Spices: Turmeric and ginger have natural anti-inflammatory properties.
-
Avoid processed foods, excess sugar, and saturated fats, as they may trigger inflammation.
Living with Rheumatoid Arthritis
Living with RA requires a holistic approach. Patients should:
-
Follow treatment plans consistently to prevent flare-ups.
-
Stay active but avoid overexertion to maintain joint mobility.
-
Use assistive devices if needed to reduce strain on joints.
-
Prioritize mental health through counseling, meditation, or support groups.
-
Monitor health regularly with their rheumatologist to adjust treatment when necessary.
Future of RA Management
Ongoing research continues to explore new therapies for RA. Advances in biologic drugs, stem cell therapy, and personalized medicine show promise in improving long-term outcomes. With early detection and proper management, many patients can now live productive, active lives despite the disease.
Conclusion
Rheumatoid Arthritis is more than just joint pain—it is a complex autoimmune disorder that can impact the entire body. Early diagnosis, timely medical intervention, and lifestyle adjustments are essential for controlling the disease and preventing complications. While RA may not be curable, advances in medicine and patient-centered care have transformed it from a disabling condition into one that can be effectively managed.
For those living with RA, knowledge is power. Understanding the condition, recognizing symptoms early, and seeking expert medical advice can make a significant difference in leading a healthier, more fulfilling life.